Making It Count
In a few of my blogs you’ve probably read a little about counting, and hopefully you grasped that it is a big deal! But why is it such a big deal? In most surgical procedures there are a lot of items opened that could easily be lost if not accounted for. There are a lot of places something can be ‘lost’ during a procedure. For example, most often the item is found on the floor, under someone’s shoe, in the trash can, stuck to another item, the list goes on. These items can also be found inside the cavity in which you are working, which is why counting is necessary. If a team follows their count policy, then there should be essentially no risk of it becoming a RETAINED surgical item, or an RSI. An RSI is a foreign object that is unintentionally retained after the procedure. A patient with an RSI could have severe complications related to whatever object that was unintentionally left inside the patient. This could be life threatening. See why it’s a big deal?
Every facility should have their own count policy that is drafted from a number of sources. AORN, AST, and an accrediting agency, such as The Joint Commission, are the typical sources for the backbone of any count policy. The policy will also outline exactly what gets counted for which type of procedure, when counts are to be performed, and what to do with a discrepancy.
WHAT gets counted?
The main groups of countable items are sponges, sharps, smalls, and instruments. Sponges consist of raytecs, laparotomy sponges, peanuts (kittners), cottonoids, and any other “sponge” that is opened. These all have a radiopaque material imbedded in them which make them traceable by x-ray if they are lost within the body. Sharps are your blades, hypodermic needles, suture, bovie tips, etc. Smalls can be a large range of objects such as penrose drains, vessel loops, suture booties, rubber bands, scratch pads, etc. Instruments include each “tool” that is opened to the sterile field. Items are counted individually (with some exceptions). Below is an example of that sequence for some basic items.
HOW to count?
When counted items are added during the procedure, they are added to the count sheet by the nurse and then accounted for during the next count. When receiving something additional to the field, it is best practice for the scrub to state what is being added for closed loop communication. For example, “Plus 1 blade” or “Plus 1, 2, 3, 4, 5, 6, 7, 8, 9, 10 raytecs” or “Plus 1, 2 Kellys”. A nurse should always be involved in the count as the licensed individual. This is documented in the EMR and by likely every policy, it’s a non-negotiable that a nurse must be involved in the count. It’s also extremely helpful when a nurse has a good knowledge of what each instrument is!
When counting make sure that the nurse is able to see each item that is counted. Also, make sure to completely separate each sponge. Raytecs come in packs of 10, which is why most facilities count by 10s, lap sponges come in packs of 5, peanuts 5, tonsil sponges 5, cottonoids 10, etc. Sponges are usually counted in the manner they are packaged, but this can differ from facility to facility. As items on the field should be separated, so should items off of the field. Once you have thrown sponges off the field into the kick bucket the circulator should hang them in a sponge counter where they are separated and easily viewable by the team. I’ve seen many techs with poor practice count sponges without separating them, and while most of the time that may not cause an issue there is always a chance that your pack of 10 raytecs was actually a pack of 9 or 11. This does happen and would easily be caught if the count is performed correctly.
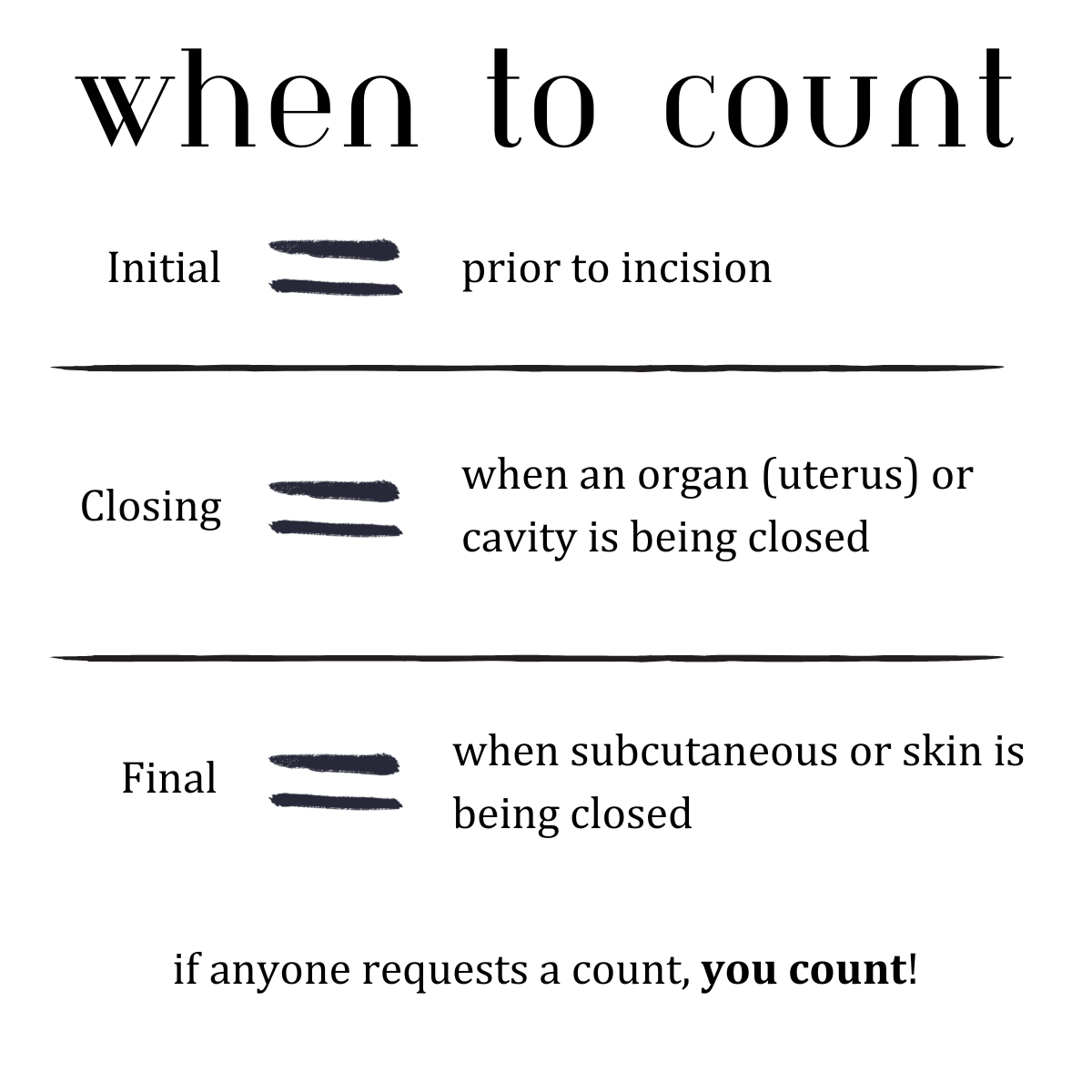
WHEN do you count?
All procedures will have a minimum of TWO counts. The initial count and the final count. The initial count should always be done before the incision is made. Some places have policies that the count must be performed before the patient is even in the room. This is doable, but it does but a strain on efficiency. Don’t forget that turnover time goal! The final count is the last count of the procedure. This count is done during the subcutaneous or skin closure. Like I mentioned, the initial and final counts are done on all procedures with countable items. Some procedures like a basic cystoscopy or a myringotomy with tubes don’t require any countable items, so there is no count.
A closing count is performed when a cavity is being closed. For example, if you are doing an exploratory laparotomy and the surgeon begins to close the peritoneum you do a closing count. In this case, the closing count is a full count.
A mesh count is performed when mesh is being inserted to ensure there is nothing remaining “under” where the mesh is being placed.
A relief count is performed with a permanent change of the circulator or the scrub, or if it’s a lunch break and the case will be finished by the time you return.
I’ve seen some scrubs try to brush of counts in little cases- not okay! Why should I count if I only have 5 tonsil sponges on my sterile field? Well, let me tell you from personal experience. One day I was scrubbing a tonsillectomy and the only countable item on my entire set-up were the tonsil sponges. These are large firm cotton ball sized sponges with about a 6” tail on them. Hard to misplace, right? The surgeon decided to pack the tonsil bed with a tonsil sponge while the patient awoke from anesthesia- while he says he communicated with the team that was his plan, no one heard him! And, if you’ve ever worked with an ENT surgeon, you know a tonsillectomy can be SUPER fast so you’re usually counting as the surgeon says “okay, I’m done” since there is no wound closure involved. Long story short, I started the final count and only found 4 tonsil sponges. The patient wasn’t awake yet and the surgeon was still in the room. The nurse and I started QUICKLY looked around for the 5th sponge and did not see it. While we are looking, we tell the surgeon we only have 4 of the 5 sponges. He calmly says, “I know, I put it in the tonsil bed until he’s extubated.” We lose our panic mode, luckily. At the last minute he had grabbed a sponge off the mayo without me seeing and snuck it in. Packing the tonsil bed during emergence is a common practice so prevent bleeding, and it is to be pulled out WITH the endotracheal tube. However, usually there is clear communication between the surgeon, scrub tech, nurse, and anesthesia to prevent an RSI. Moral of the story, if I wouldn’t have done a final count JUST for those 5 tonsil sponges, the patient would have been wheeled out of the OR with a tonsil sponge in the back of their throat if no one had caught it beforehand. No matter how silly or small it seems, do the count!
What if there is a discrepancy?
In the event of a miscount, immediately notify the surgeon. That way they can be on the lookout for the missing item as well. No surgeon wants to hear that you’ve been looking for a lap sponge for the last 3 minutes when they’ve been closing the peritoneum, speak up!! Keep searching for the item. The tech should be searching on the field while the nurse searches off the field until the item is either located or there is a decision to call x-ray. Open up and shake each sponge on and off the field to ensure it did not get stuck to another sponge. Go through the trash! I cannot tell you how many times I’ve found what was missing in the trash can! Not pointing fingers, but some people who break mid-procedure sometimes have items in their hand, like sponges, and just discard them with their gown and gloves. So, let’s say you’ve looked without success, now it’s time to call x-ray to come and take some images to see if the item missing is in the surgical wound or not. While you’re waiting on them- keep looking! I’ve found items many times between the time x-ray was called and the time they arrived, saved us all some radiation! Each facilities policy when it comes to a discrepancy is likely a little different, but you should always keep looking.
There are very few instances where a count can be ‘waived’. One of which is a trauma situation when the few minutes it takes to count should be spent trying to save a life- and in that case an x-ray is almost always mandatory. Another time counts may be waived is in an organ donation procedure. I personally enjoy counting; it makes me feels well organized and accomplished. No matter if you enjoy counting or not, it has to be done for the safety of the patient!