Pediatric Patients
Clinically, pediatric patients are much different that the adult population. They are also intellectually different in many ways. Within the pediatric population there are significant differences based on their age. A 1-year-old patient is very much different than a 9-year-old patient, you would not interact with them in the same ways to provide the care they are to receive. During nursing school, I tried to keep an open mind to other specialties, and I did enjoy pediatrics, but I did not think I could handle the terminally ill patients. I felt that I would relate everything to my own kids- I had 2 children and was pregnant at that time. I am not sure if that truly would have been the case, but I decided against pursuing a career in pediatrics. So, now in the OR I still get to interact with the pediatric patient population, but in a different way!
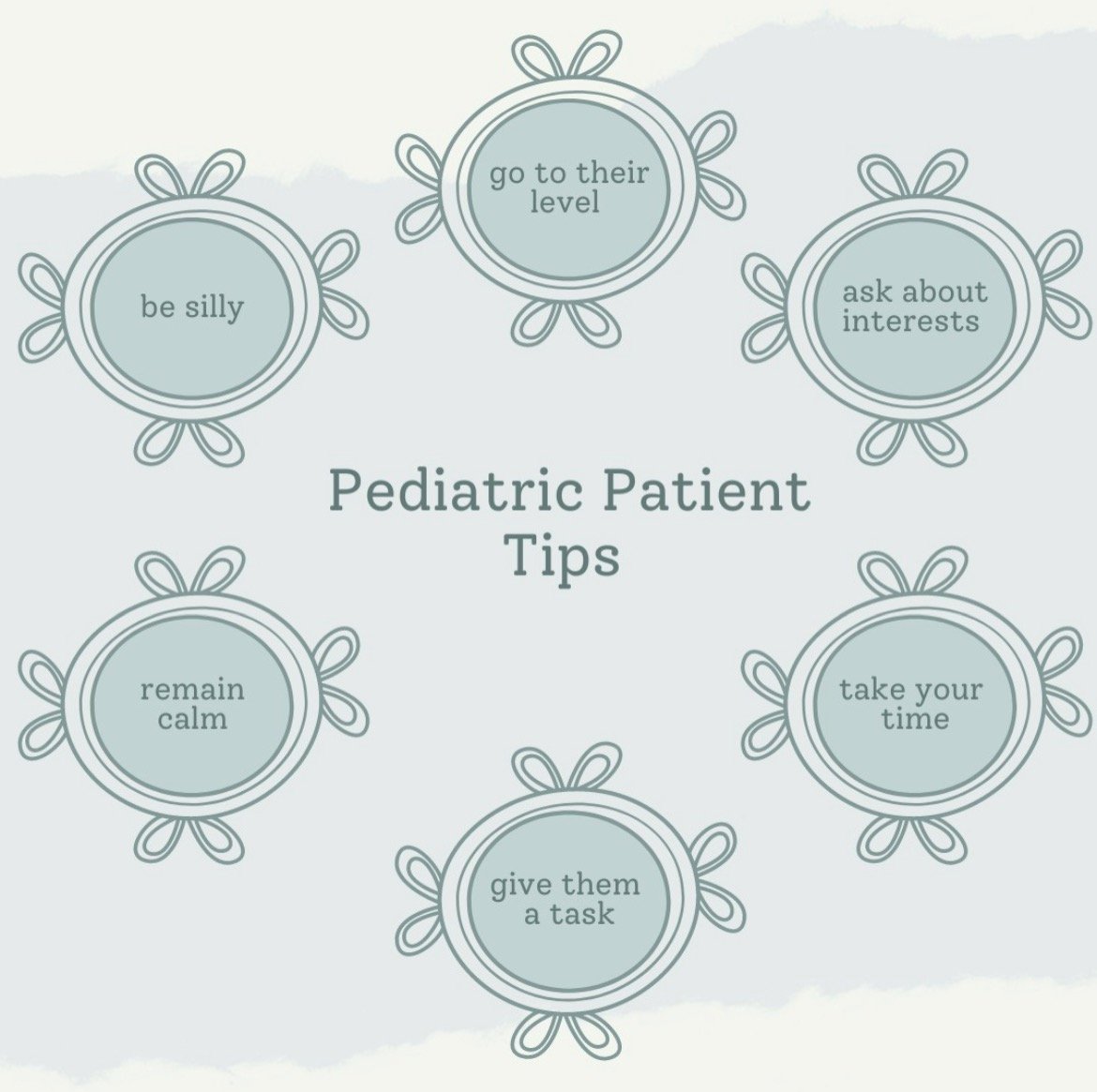
I work in ENT quite often. In this specialty, a good majority of your patients are young children. Some even babies! Pediatric patients are different clinically and have different communication needs. In my experience, the pediatric patients I have cared for are often having simple procedures performed such as myringotomy for tube placement, tonsillectomy, adenoidectomy, foreign body removals (kids shove things in their nose and ears A LOT). Here are some of my tips for getting those younger patients comfortable in that preoperative visit.
1. Get on their level
Crouch down to be eye level with your pediatric patient. Doing this will hopefully reduce feelings of intimidation they may feel. Speak to them at their level. Make it simple but stay truthful. Do not lie and set unrealistic expectations.
2. Ask about interests
Ask the patient about what they like. Do they like dogs? Princesses or superheroes? If they have a stuffy with them, ask what their name is! Find something you can chat with them about and keep them talking. If your patient isn't opening up, then see if their parents/caregivers may give you a few tips on what they may be interested in talking about. A lot of shyness disappears when a patient starts talking about something they are interested in.
3. Take your time
No one like to be rushed. Especially children, if you're a parent you are well aware of this! Make sure you head down to pre-op a few minutes early to give yourself that time to make a connection and to avoid rushing. The patient will likely be more cooperative if you take that much needed time. Plus, the parents/caregiver will be thankful for a nurse that took that time to make that connection. I say take your time, but also be efficient to keep the day moving!
4. Give them a task
Ask them to hold something for you on the trip. I like to ask then to hold the blood pressure cuff, AKA muscle tester, on the way. This gives them something that they can feel in control of. Make a big deal about it for them, act like there is no possible way you could have gotten it to the OR.
5. Remain calm
Children, and their parents, will pick up on your behaviors and actions. Keeping calm will help the patient feel more comfortable and will likely leave the parent/caregiver more at ease about the procedure.
6. Be silly
Make them laugh! Don't be afraid to do something goofy to get them to laugh. Sing songs with them. Pretend that the bumps on the way down are part of a crazy rollercoaster, tell them to hold on tight! Let them push the button to open the magic doors. Make their stuffy match them, give them a hat and a mask! Take advantage of the trip from pre-op to the OR and talk about the cool big lights on the ceiling and all of your friends that are going to be there to help take care of them. Tell them about the nice warm blanket you have waiting for them when you get there.
A lot of times they will bring a comfort item from home, like a stuffed animal, blanket, pacifier, etc. Ask if they would like to bring their stuffy along for the ride, comment on how cool their blanket is! Let them bring a comfort item or two with them when you go to the OR. They’ll be separating from their parents, so this item will hopefully be the piece that keeps them comfortable during this experience which may cause a wide range of emotions. It’s always easy to bring a kid back who is more than willing to jump in your arms to be carried or ride on the cart, but it feels like for every easy kid you get two challenging ones in return! It makes sense, most parents teach their children not to speak to strangers, right? Talk with their parents, build some rapport with them in front of the child and with any luck the trust you build with the parents will be felt by their child and will make things a little easier. Unfortunately, there will always be the children that go back kicking and screaming. It sucks, but it is in an attempt to improve their health.
As you drop the parents off in the waiting room, you’ll have to decide what kind of ‘good-bye’ will be best suited for the patient. Some kids are unbothered and will look at their parents and wave bye to them like it’s a normal day, others not so much. Sometimes we don’t have an actual ‘stop and say our goodbyes’. Sometimes I talk with the parents, and we decide it’s best to just keep moving because stopping to say bye would make it more difficult for the patient. Sometimes the patient doesn’t even realize that the parents stayed behind. Pay attention to the patient’s verbal and non-verbal communication to see what might work best.
Once I get into the OR I always talk about all of my friends that are going to help take care of them. The scrub will usually be waiting at the side of the table with a warm blanket to help encourage the patient onto the operating table. I like to point out the OR lights and talk about how cool they are, a lot of times the patient will fixate on them, and they look a little scary, especially when they lay back, so I just make a point to talk about how cool they are, and it usually works pretty well. While you’re in the OR you want to keep the patient as under stimulated as possible. It’s best for only one person to be talking with the patient at a time, usually that’s the nurse and the CRNA or a combination of the two. I am usually the one doing the talking until the patient gets over to the table, then the CRNA will take over the conversation. I still remain at the patients side the whole time until the patient is anesthetized and properly “restrained” to reduce the risk of falling off the bed.
While working with the pediatric patient population may or may not be your thing, I hope you were able to take something from this and apply it to your interactions!